Health Communication In Southern Africa ~ Using Pictograms In A Patient Information Leaflet To Communicate Antiretroviral Medicines Information To HIV/AIDS Patients In Rural South Africa
Abstract
The objectives were to design a simple, illustrated patient information leaflet for the antiretroviral regimen of stavudine, lamivudine and efavirenz and to evaluate its readability and acceptability in the local Xhosa population. In order to achieve this, a further objective was to design and evaluate illustrations to include in the patient information leaflet which were culturally acceptable and well interpreted. Illustrations or pictograms were designed to illustrate selected instructions appearing in the patient information leaflet and were individually tested in 30 Xhosa participants who had a maximum of 8 years of formal schooling. Results were used to improve the pictograms for inclusion in the patient information leaflet. The patient information leaflet was designed and tested in sixty Xhosa participants with varied levels of education who had stated they could read. Demographic data were collected and they were then asked to read the patient information leaflet, available in both English and isiXhosa, and a series of questions was asked to assess its comprehension and acceptability. The overall average rate o f understanding was 95. Six of the 20 questions were located and understood by all participants, and only two questions resulted in less than an 85 correct response. Physical appearance and quantity of information were highly rated and all participants were enthusiastic about the inclusion of pictograms.
Introduction
The communication of health-related information in Africa has involved various media including theatre (Mbizvo, 2006), video (Mathews, 2002), television and radio (Health Communication Partnership, 2008) and folk media which includes poems, dance drama, story-telling, rhymes and sayings (Gokah, 2007). However, the most commonly employed method has been the use of print media (Peltzer, 2002). Low literacy rates coupled with inadequate infrastructure and poor technological development in African countries have favoured the use of posters, billboards and pamphlets for health promotion and patient education.
Medicine-taking behaviour is complex, multi-factorial, and depends on a dynamic interaction of several factors, including cognitive, behavioural, social, environmental and physiologic factors (WHO, 2003). A minimum requirement for using medicines safely and effectively is a basic understanding of the medicine instructions and the ability to recall this information. However, the communication of this information to the average patient in southern Africa presents a complex challenge to health professionals as poorly resourced health care systems result in minimal time spent with individual patients and the cultural, educational, socioeconomic and linguistic differences that often exist between health professionals and patients may further challenge successful communication. Limited reading skills, a poor knowledge of the body and its systems and inadequate insight into diseases and their treatment also disadvantage patients seeking to address their health problems.
Traditionally, much health and medicine-related information has been communicated verbally, which is congruent with the strong oral tradition in Africa, but this has its limitations as patients tend to forget half of what they hear from the doctor within five minutes of leaving the consultation room (Kitching, 1990). The use of written materials for informing and educating patients on health issues and medicines has increased substantially over the years, albeit mainly in the developed world, with the patient information leaflet being the most widely used form (Kenny et al., 1998; Raynor et al., 2007).
Patient information leaflets communicate more information than can be achieved by counselling alone and have been shown to be beneficial in improving patient understanding and knowledge of their medicines, enhancing recall of instructions, reducing medication errors along with patient anxiety about treatment, bridging the information gap between patients and healthcare providers and improving adherence to medicines (Johnson 2005; Kitching, 1990; Koo, Krass & Aslani, 2003; Mansoor & Dowse, 2006; Raynor, 1998). However, in order to fulfil its potential, the form and quality of written information must match the reading level of patients and should take into account their culture, beliefs, attitudes and expectations (Doak, Doak & Root, 1996; Schaafsma, Raynor & de Jong-van den Berg, 2003).
Irrespective of educational level, people generally prefer simple and easy-to-read materials and find it easier in the clinical situation to comprehend and act appropriately on short, simple messages than on more complex ones (Doak et al., 1996; National Work Group on Literacy and Health, 1998). Therefore, information intended for patients should be written in the simplest form possible for optimal acceptance and comprehension, particularly if a high proportion of the target population has limited literacy (Davis et al., 1994; Mansoor & Dowse, 2007).
For a number of decades, health education in Africa and other emerging countries has included the use of visual aids (Hugo & Skibbe, 1991; Kwansa, Cannon, Belcher, & Hosu-Porbley, 1972; Linney, 1995; Zimmerman, 1982). Visuals have been shown to enhance the understanding and recall of medicines information, particularly for patients with limited health literacy skills (Doak et al., 1996; Mansoor & Dowse, 2003; Dowse & Ehlers, 2005, Houts et al., 2006; Katz, Kripilani & Weiss, 2006; Ngoh & Shepherd, 1997). A common assumption often reported in popular literature is that visuals constitute a universal language which can be easily understood by all, regardless of culture, language, beliefs, or education. However, cross-cultural testing of visuals has clearly shown that pictures do not necessarily communicate the same concepts to all groups, even when the pictured objects are easily recognizable (Dowse & Ehlers, 2001; Doak et al., 1996; Tripp-Reimer & Afifi, 1989). Visual materials for health education are often designed by health professionals and graphic design specialists who may lack adequate insight into the culture and the visual literacy skills of the target group and adopt a top-down approach of “we know best” in the design process. On the contrary, the optimal approach in designing culturally sensitive, content-applicable visuals is to involve the target group in all stages of the design process, and to test the final image rigorously in the target population before it is included in any type of patient information materials (Dowse & Ehlers, 2001).
The high incidence of HIV/AIDS in South Africa is well documented, with an
estimated 18.8 of the adult population being affected (UNAIDS, 2007). AIDS is a chronic condition with no cure, but it can be managed with combination therapy using a minimum of three antiretroviral drugs concurrently. This chronic, complex therapy demands extremely high adherence levels of more than 95, as poor adherence has been associated with the development of resistance and ultimate therapy failure (Gardner et al., 2008). Patients initiated on antiretrovirals receive an enormous amount of information at a time when they are physically and emotionally vulnerable, and they are expected to adhere to a complex medication regimen which often results in distressing side effects. Written patient information materials may be of particular value for these patients when a large volume of information is communicated verbally, as it serves to reinforce the verbal information and act as a permanent source of reference and as aid to the recall of information.
Over the past two decades, growing evidence has revealed the magnitude and consequences of limited literacy on the health and health care of many at-risk patients. Literacy has been reported as a stronger predictor of health than level of education, being linked to delays in accessing and using preventive services, adherence to medical instructions, compromised self-care skills and poorer health outcomes (Davis & Wolf, 2004). The most recent census conducted in South Africa in 2001 reports that 22.8 of the adult population have no schooling, and a further 19.8 have only “some” primary school education (Statistics South Africa, 2001).
From these figures, approximately 43 of the population may have compromised literacy skills, with this same proportion therefore likely to encounter some difficulty in reading and comprehending written health information. The problem is exacerbated by this information often using language at a higher level than the average reading level of the patient (Doak et al. 1996; Kenny et al. 1998).
In South Africa, the provision of patient information leaflets with all medicines was mandated by Regulation 10 of the Medicines and Related Substances Control Act, Act 101, as amended, from May 2003 (Government Notice, Department of Health, 2003). This regulation requires the pharmaceutical industry to develop and distribute patient information leaflets with all their manufactured medicines. Although antiretrovirals supposedly received high priority in this initiative, to date there is little evidence that these patient information leaflets are being distributed from public sector hospitals to patients receiving antiretrovirals. This project attempts to address the lack of written information available to patients receiving antiretrovirals.
Research objectives
The objectives of this research were to design a simple, easily readable, illustrated patient information leaflet for a commonly used antiretroviral regimen, and to evaluate its readability and acceptability in the local Xhosa population. In order to achieve this, a further objective was to design and evaluate illustrations to include in the patient information leaflet, which were culturally acceptable and well interpreted.
Method
Study site and study population
The two studies described in this chapter were both conducted in Grahamstown, a small town in the Eastern Cape province. This is one of nine provinces in South Africa and is largely rural, underdeveloped and economically poor, with a high unemployment rate. The majority of the local black population belongs to the Xhosa ethnic group, and it is from this group that the participants in this study were drawn.
Participants were recruited from a number of sites within Grahamstown; Settlers Day Hospital which is a primary health care clinic, a local community centre and the suburban areas adjacent to the community centre. Interpreters, who were used for all interviews and group discussions, received individual training and were subsequently evaluated during practice interviews. All participants received an honorarium in acknowledgement of their time. Approval for the study was obtained from the Rhodes University Ethical Standards Committee.
Development of pictograms
Seven pictograms to be included in the patient information leaflet were identified. Five of the pictograms had been developed and tested by the author and co-workers (Dowse & Ehlers, 2001). For the design of two new pictograms, a workshop was conducted with the second year undergraduate Pharmacy class at Rhodes University. Students in this class represented 15 African countries, including the study target population. Background information on the design and use of pictograms as well as the problems associated with their interpretation were presented. Students were then split into groups of between 5 and 8 and were presented with two instructions to illustrate: “Keep medicines out of the reach of children” and “Store medicines in a cool, safe, dry place away from heat and direct sunlight”.
The visual concepts and rough sketches generated from this workshop were discussed with a graphics designer who produced initial versions suitable for testing. A group discussion with five Xhosa participants guided the modification of both the initial images of the two new pictograms as well as the existing pictograms. Of the seven pictograms which were to be included in the patient information leaflet, three of these were direct instructions to take the medicine either once or twice daily. Only the “twice daily” pictogram was tested. Ten pictograms in total were tested, five of which were to be included in the patient information leaflet. The remaining five had been tested in previous studies (Dowse & Ehlers, 2001) and were included to contribute to the internal validity of the study, as results could be compared with existing data collected from a similar population. Only results for the five pictograms included in the patient information leaflet will be presented and discussed (see Appendix).
Testing of pictograms
For inclusion in the study, participants had to be 18 years or older, and have a maximum of 8 years of formal schooling. Thirty Xhosa participants were recruited with the help of an interpreter, who provided a brief, scripted explanation about the application of the pictograms followed by a discussion of two examples of pictograms to familiarise participants with the concept.
In individual interviews, demographic data were collected (sex, age education) and the ability to tell the time either from a clock face or a digital display was recorded. The pictograms were then displayed in random order, one at a time, and participants were asked to offer their interpretation. Responses were recorded as correct or incorrect and all comments were noted. Participants were thanked and were given a small monetary donation in acknowledgement of their time and input. Interviews took between 15 and 30 minutes. The criterion used for acceptance of the pictograms was the American National Standard’s Institute ANSI Z535.3 which advises that, in a comprehension test, pictorial symbols must reach at least a criterion of 85 correct (ANSI, 1991).
Development of the patient information leaflet
Information on the antiretrovirals constituting Regimen 1a (stavudine, lamivudine, efavirenz) used in the South African public health sector was collected and consolidated into one written leaflet. The patient information leaflet was designed to comply with most of the local legal requirements stated in Regulation 10 (Government Notice, Department of Health, 2003).
The design of the patient information leaflet was informed by published guidelines on patient information design (Koo, Krass & Aslani, 2003; Sless & Wiseman, 1997) with particular attention to designing for readers with limited reading skills (Doak et al., 1996, PATH, 2002). All information was carefully considered for its relevance, and concerted attempts were made to minimise medical jargon and avoid the use of complex, multi-syllable words rather including simple, easily understood words.
A three-column format was adopted and an easy to read font in an appropriately large font size (Arial 10 point) was used for the text. Large, dense blocks of text which are intimidating to poor readers were avoided by breaking the text into short blocks, and frequent use was made of bullet points to simplify and emphasise multiple points of information. Sentences were kept short and active voice was used throughout. Navigation through the leaflet was facilitated by using headings which were emphasised using a bold, larger font size and were bordered with a line above and below the text. The inclusion of adequate white space to enhance reader appeal was considered. The pictograms were included to illustrate selected information presented in the text and to promote the understanding of these points. The resulting two-page A4 size patient information leaflet was subjected to Fry’s readability test (Doak et al., 1996) which allows a quick estimation of readability levels, and was found to be suitable for Grade 7 learners.
A pilot study using 20 Xhosa participants was conducted to test the first version of the patient information leaflet in English and to refine the questionnaire. Minor modifications were made to the content and layout of the patient information leaflet and certain questions were simplified for easier translation. The final version of the patient information leaflet (Mwingira & Dowse, 2007) was then translated into isiXhosa using a multistage approach of translation by a professional translator, followed by professional proofreading and subsequent back translation.
Testing of the patient information leaflet
Inclusion criteria for participants included a stated ability to read (at even a very basic level) in either isiXhosa or English, to be 18 years or older and to have attended a local clinic and received medication for any condition. Participants were not HIV/AIDS patients receiving antiretrovirals. A standard approach was used for all the interviews in which potential participants were first asked if they could read. If the reply was positive, they were invited to participate and were told that the study aimed to assess the quality and usefulness of the patient information leaflets, rather than to test their reading skills.
Selected demographic data were collected (gender, age, home language,
educational level). Participants were then handed the patient information leaflet, with a choice of reading either the English or isiXhosa version, and were asked to read through it at their own pace. The time taken to read the patient information leaflet was discreetly recorded using a stopwatch.
In the first stage of the testing process, understanding of the pictograms was
assessed. Participants were asked to study each pictogram included in the patient information leaflet and offer their interpretation of each one. Responses were recorded as correct or incorrect and all comments were noted.
The second stage involved evaluating understanding of the text-based information and was based on that pioneered by the Communication Research Institute of Australia (Dickinson, Raynor & Duman, 2001, Sless & Wiseman, 1997), whereby participants were asked a series of 20 questions. Each question was simply worded, related directly to information presented in the patient information leaflet and required no inferences or application of prior knowledge. Questions were asked in two parts; firstly, participants were required to locate the appropriate information in the patient information leaflet pertaining to the question asked and to point this out to the interviewer, or to acknowledge that they were unable to do so. Secondly, they were asked to explain that information in their own words so as to evaluate comprehension as the ability to read the text does not necessarily ensure good understanding of the meaning. Participants had unlimited time to access and read the information before answering. Answers were recorded in two categories of “located” and “understood”. Understanding of the information was calculated according to the number of answers correctly located and explained.
Acceptability and participant opinion of the patient information leaflet were then investigated by asking a number of set questions as well as encouraging open-ended feedback. At the conclusion of the interview, participants were thanked and were offered a small honorarium in acknowledgement of their time and contribution to the study.
Data analysis
The percentage correct interpretation for each pictogram was calculated. An understanding score for the patient information leaflet was calculated based on the number of questions answered correctly. Understandability was assessed using the European Commission (EC) guideline (Dickinson et al., 2001) which sets a target that at least 80 of the participants correctly answer each question, in that they should both locate the appropriate information and be able to explain it in their own words.
Results
Pictogram study
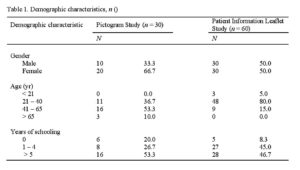
Demographic results are presented in Table 1. Of the 30 participants interviewed, 20 (66.7) were female and 10 (33.3) were male, and all had isiXhosa as their first language. A majority (53.3) were between 40 and 65 years of age. Six (20) of the participants had not received any formal education and 16 (53.3) had between five and 10 years of formal education. Twenty-eight of the 30 participants could tell the time from a clock face.
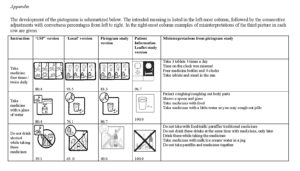
The Appendix shows various stages in the progression of pictogram development. The USP pictograms, which are designed mainly for use in the United States (USP, 2000) were the original starting images for all our pictogram development work. The “Local version” pictograms are the images we developed by modifying the USP pictograms, with their development, testing, interpretation and misinterpretation having been previously reported (Dowse & Ehlers, 2001; Dowse & Ehlers, 2004).
Results from these two stages (USP and Local versions) have been included as they informed the current development process reported in this study. Examples of misinterpretation of each pictogram found in this study are displayed in the Appendix. The “Take medicine four times a day” pictogram was well interpreted but narrowly failed to meet the 85 ANSI criterion. The ideas from this pictogram as well as from a pictogram showing a “take at night” instruction (Dowse & Ehlers, 2001) formed the basis of the “Take medicine twice daily” pictogram included in the patient information leaflet. A dark background was used to convey the concept of night time, with a sleeping person on a bed and a moon included to reinforce the time of day. The times to take the medicine would be filled in by the health professional on the clock face. Only two of 60 participants failed to correctly interpret the version of the patient information leaflet.
Although the pilot study pictogram “Take medicine with a glass of water” complied with the ANSI 85 criterion, participants found the insert with the profile confusing and it was deemed to be superfluous. They also commented negatively on the lines depicting movement in a liquid, which were subsequently removed. The capsules and tablets were modified to more closely resemble those used in practice. The final version of the patient information leaflet was understood by all participants.
Certain images in the “Do not drink alcohol while taking these medicines” pictogram were considered to be outdated, as containers such as the carton, which was previously widely used for beer, are no longer available. The carton image was replaced by a larger, popular beer bottle. The short, stout bottle was taken to resemble a milk bottle, which resulted in it being modified to a more slender, longer bottle. The lack of text on the labels elicited comments that the bottles could contain any liquid, so the word “Beer” was included on the label. The shape of the mug was modified and increased in size. Finally, the bottles were repositioned to increase their visibility below the cross, which was drawn as a solid cross extending to all four corners of the image box. From a very poor interpretation of 40, the final version of the patient information leaflet resulted in 100 understanding.
The pictogram describing storage conditions was totally redesigned as the USP and the Local versions only illustrated the instruction “Do not store near heat or in sunlight” and the interpretation of both versions was particularly poor. For storage of antiretrovirals, patients were encouraged to not only avoid any sources of heat, but also to store their medicines in a cool, dark place which was illustrated as a shaded cupboard interior. Various versions of the sun and the fire were informally tested on 5 local Xhosa people. The pilot study version was adequately interpreted, but failed by a fairly large margin to reach the ANSI 85 criterion. The image of the sun was variously described to look like the moon, a clock face, a broken tablet, whereas others failed completely to recognise it. Comments on the fire included “looks like a tree with leaves” and “a lit cigarette ready to be smoked”. The pictogram was modified to centre the sun in the circle, remove the smoke from the fire, include a solid black cross, and the shape of the cupboard was altered to one that looks more like a cabinet, with the size of the medicine packet being increased and the bottle image removed.
The final pictogram “Keep all medicines out of the reach of children” used the USP version as a starting point, with the initial image from the graphics designer shown under “Local version”. This was never tested and was designed for the current study. Following comments from the group discussion, it was modified to include an adult and a small child, and a cupboard similar to that used in the storage pictogram was added. This achieved a 90 correct interpretation and was subsequently modified only to change the look of the cabinet to ensure a degree of uniformity with the storage pictogram. Interpretation of all five pictograms improved following modification, when they were included in the patient information leaflet and tested during the final study.
The study of the patient information leaflet
Males and females were evenly distributed for this study (Table 1), and the average age ranged between 21 and 40 years (80). Five participants (18) had less than five years of formal education. Just under half (47) had attended school for more than 10 years, with many of these having also achieved some form of tertiary education.
Participants took an average of nine minutes to read the patient information leaflet, with only three participants reading it in under 5 minutes. Most of the information in the patient information leaflet was well located and understood (Table 2) which is reflected in an average overall rate of understanding of 95. The answers to six of the 20 questions were located and understood by all 60 participants. The target set by the EC guideline that at least 80 of participants should answer each question correctly was achieved for 18 of the 20 questions. The most challenging question (Question 3) related to the possibility of developing resistance if medicines were not taken as instructed as only 40 of the participants were able to correctly explain the meaning of the text. A high degree of adherence to antiretrovirals is the cornerstone of managing HIV/AIDS and insight into the potential negative outcomes of poor adherence is crucial. The patient information leaflet therefore requires further modification to make this information more conspicuous and understandable.
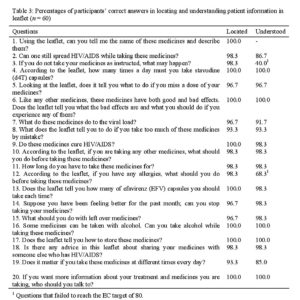
Table 2: Percentages of participants’ correct answers in locating and understanding patient information in leaflet (n = 60)
The other question that failed to meet the EC target dealt with allergies and taking antiretrovirals (Question 12). As with Question 3, this is a complex, two-part question, firstly requiring the participant to identify with a condition i.e. experiencing an allergy, and thereafter requiring an understanding of the consequences of not obeying an instruction. In both cases, location of the information was excellent, but participants were unable to understand and use the located information to inform their own medicine-related behaviour.
Acceptability of the patient information leaflet
Interestingly, 18 of the 60 Xhosa participants chose to read the English version of the patient information leaflet, even though they were literate in isiXhosa, as they were more comfortable reading English and considered the English words to be easier to understand and simpler than the isiXhosa translations.
Most participants (62) found the patient information leaflet to be of average difficulty, whereas only three of the 60 found it difficult to read, with the remaining third considering it to be easy to read. All considered the font size to be sufficiently large (100), and almost all thought the length of the sentences to be reasonable (95), and the space between the lines of text adequate (97).
The amount of information included in the patient information leaflet was considered by 88 to be sufficient to inform the appropriate use of the medicines. The presence of pictures appealed to all 60 participants who felt that the pictures would contribute to understanding and recalling the information. The level of difficulty of the words generally appeared to be appropriate as most participants (90) said that there were only a few words that they were unable to understand e.g. 83 of participants reported being unable to understand “viral load”, 85 had difficulty with “CD4 count” and 87 reported difficulties with understanding “antiretroviral therapy”. Other words included “resistance” (12 misunderstood), “pharmacist” (10 misunderstood) and “capsules” (5 misunderstood). Participants appreciated having a choice of language in which to read the patient information leaflet. Forty-four of the 60 (73.3) stated that they would prefer to receive patient information leaflets in their home language of isiXhosa.
The product description section at the end of the patient information leaflet elicited many negative comments and was not understood or liked by the majority of participants. In their opinion, it did not constitute important or relevant patient centred information, was too technical and was of no value in informing medicinetaking behaviour.
Discussion
The design and development of the pictograms and the patient information leaflet were iterative, multi-stage processes informed by established design guidelines and involved members of the target population at all stages of development and testing, thus ensuring cultural acceptability and an appropriate level of complexity. The high levels of understanding for both the images and the written text, as well as the positive opinions of the patient information leaflet reported in this study provide evidence of the success of this strategy, supporting previous research using this approach (Doak et al., 1996; Mansoor & Dowse, 2003).
The benefit of improved comprehension and high acceptability when incorporating visuals into written medicines information intended for a low-literate South African population has been shown by Mansoor & Dowse (2003), and is supported by the findings in the current study. The pictograms all illustrated concrete concepts and direct instructions which are easier to both represent and to understand than abstract concepts and feelings. The images were drawn as simply as possible, with clean lines, avoiding all unnecessary extraneous details. This strategy attracts the eye of the viewer directly to the core, central concept of the image rather than have the viewer randomly focus on distracting detail and reduces the cognitive load on the viewer, particularly relevant in those with poor visual literacy skills (Carstens et al., 2006). The majority of the images contained analogical objects i.e. familiar objects such as a glass, a cupboard, a bed, a fire, and the illustrated instructions were all familiar activities, both of which contributed to the high levels of interpretation.
Attempts were made to avoid the use of graphical conventions and symbols e.g. arrows, which require higher order symbolic interpretation strategies (Maes et al., 2008). An arrow had originally been included in the circular insert of the Pictogram Study version of “take medicine with a glass of water” and was intended to show the action of moving the glass towards the mouth, but was completely overlooked by many participants. Following testing, the insert was identified as an unnecessary source of confusion and was therefore removed in the study of the final version of the patient information leaflet.
The importance of including representatives of the target culture in all stages of testing was clearly apparent with the “Avoid alcohol” pictogram. Early work on the USP version (Dowse & Ehlers, 2001) clearly showed that representing different types of alcoholic beverages by showing various shapes of glasses was meaningless in this population. An added problem was the use of the single slash, a graphical convention used widely in road signs, to denote a “do not” instruction, which was then changed to a negation cross. The many subtle changes made to the bottles and the mug which resulted in a successful final version were only possible as a result of insight offered from participants of the same culture.
The improved interpretation of the pictograms when presented in a combination text-image format (version used in the study of the patient information leaflet) possibly resulted from viewers being better able to contextualise the image within a body of information which provides an automatic prompt to the viewer in creating meaning from the image. Another reason is the generally higher level of education of participants in the study of the patient information leaflet, as all participants were required to possess literacy skills, unlike many of the targeted low literacy participants in the Pictogram Study.
Information leaflets should stimulate the interest of the consumer, and should be user-friendly, attractive, informative and easily readable. Consumer testing, in which consumer preferences are evaluated via open-ended questions, is the best way to assess this and forms an important part of the design process of patient information leaflets (Dickinson et al. 2001). This study employed a combination of open-ended and closed questions to ascertain opinion and preference, a process which was invaluable in informing the modification of the document and optimising its physical appearance and readability.
The lack of understanding of the words “antiretrovirals”, “CD4 count” and “viral load” may seem surprising, given the prevalence of HIV/AIDS in this country. However, this study was conducted at a time when the availability of antiretrovirals to patients in the public health sector was still severely limited. In addition, participants in the study were not taking antiretrovirals and were unfamiliar with the disease. It is anticipated that almost all patients on antiretrovirals would now be familiar with these words.
South Africa has 11 official languages, which complicates the distribution of “one-size-fits-all” information written in only one language. In accordance with previous findings (Mwingira & Dowse, 2007; Schaafsma et al. 2003), participants in this study strongly supported patient information leaflets being available in the patient’s language of choice, sending a clear message that such materials must be prepared in a variety of languages to satisfy the linguistically diverse South African population. African languages have a strong oral tradition and many modern medical terms have not been directly translated. This creates problems in preparing a written translation of these leaflets as a single English medical term may need to be described using a number of less specific, descriptive African words. This may partially account for almost a third of the participants choosing to read the English version. However, these participants were generally better educated and would therefore have had more experience with reading English texts.
Most industry-generated patient information leaflets are written according to a closely controlled format legislated by national guidelines with minimal deviation being allowed. Although considerable effort is involved in developing such materials, their design mostly reflects a top-down health professional and/or manufacturer perspective rather than a patient-focused approach, and may not adequately cater for patient-related factors such as health literacy level, culture, health beliefs, needs and opinions. In a recent systematic review, Grime, Blenkinsopp, Raynor, Pollock and Knapp (2007) noted that patient experiences were seldom incorporated in written medicines information. Patients queried the independence of information produced by the pharmaceutical industry with their vested interests, feeling that the content of the leaflets was dictated more by medicolegal issues than the needs of the patient.
In May 2004, the South African Medicines Control Council (MCC) published the first version of a document entitled “Guideline on the Requirements for Patient Information Leaflets” (Medicines Control Council, 2004). The guidelines require the inclusion of information such as the proprietary name, the composition of the medicine, interactions, presentation and description of packaging material, description of physical appearance of the table, registration number of the medicine and the verbatim inclusion of certain statements pertaining to areas such as pregnancy and side effects amongst others. One of the requirements was a product description section, which appears at the end of the experimental patient information leaflet. In accordance with the findings of Grime et al. (2007), this section elicited a general consensus of being too technical and of little value to patients. In fact it was considered to be an important negative factor in that it adversely increased the overall length of the patient information leaflet and created unnecessary anxiety as readers were unable to relate this information to their own medicine-taking experiences.
The patient information leaflet in this study did not include all the legal requirements, although this was the original intention, as it would have resulted in an unacceptably long document. When designing materials such as these, user opinion and user reading ability should be taken into account by regulatory bodies when deciding on essential drug-related information. This is particularly relevant for important and potentially dangerous products such as medicines. Despite attempts to simplify and shorten the patient information leaflet, we were constrained by trying to satisfy many of the local legal requirements.
The MCC guidelines inform the developers of patient information leaflets on their content, format and readability but there is no requirement for evaluation of the final product prior to distribution and it is uncertain whether patient information leaflets developed using these guidelines will appropriately cater for the enormous diversity of the South African population.
The industry generates individual patient information leaflets for each antiretroviral, meaning that patients would receive three different leaflets for their triple therapy antiretroviral regimen, a volume of information likely to challenge even the most accomplished reader. A much more sensible approach is to produce a leaflet for each official three-drug regimen used in the public sector. Currently in South Africa, patient information leaflets do not appear to be included in the commercial medicine container for all antiretrovirals. When it is included, it is usually attached to the “package insert” which is information intended for health professionals, and is meant to be torn off and distributed to patients. This is a timeconsuming, unwieldy process and there are problems with this information, including the thin quality of the paper, the small size of the font, the reading level of the text, and the layout, all of which are factors detracting from the usefulness and readability of such information in a population with limited reading skills.
Conclusion
Written medicines information is currently not being distributed to South African HIV/AIDS patients, despite regulations mandating this process. Given the need for optimal self-care and medicine-taking behaviour in these patients, an urgent need exists for written information that is comprehensive yet simple and readable, and it should be available at all health care sites. This study showed that medicines information designed and tested according to good practice guidelines, taking patient characteristics into account, was successful in communicating essential medicinerelated information. Medicines information should be designed specifically to cater for our diverse local population and should take into account the widely varying reading skills and cultures of the South African population, it should be available in the first language of the patient and should include visuals to enhance the appeal and user-friendliness of the material. All information intended for patients should be tested in the target group before distribution. The approach to designing and developing the visuals and the patient information leaflet used in this study forms a sound basis for extending the work to additional drug groups and to other African populations.
Acknowledgements
Thanks to Rhodes University and Wyeth South Africa for financial assistance, Ms Betty Mwingira for assisting in materials development and data collection, Professor Sarah Radloff for statistical testing and all study participants for their time and intellectual input.
References
American National Standard Institute (1991). Accredited standard on safety colours, signs, symbols, labels, and tags. (Z535.1-5). Washington, DC: National Electrical Manufacturers Association.
Carstens, A., Maes, A., & Gangla-Birir, L. (2006). Understanding visuals in HIV/AIDS education in South Africa: Differences between literate and low-literate audiences. African Journal of AIDS Research, 5(3), 221-232.
Davis, T.C., Mayeaux, E.J., Fredrickson, D., Bocchini, J.A., Jackson, R.H., & Murphy, P.W. (1994). Reading ability of parents compared with reading level of pediatric patient education materials. Pediatrics, 93(3), 460-464.
Davis, T.C., & Wolf, M.S. (2004). Health literacy: Implications for family medicine. Family Medicine, 36(8), 595-598.
Dickinson, D., Raynor, D.K., & Duman, M. (2001). Patient education leaflets for medicines: Using consumer testing to determine the most effective design. Patient Education and Counseling, 43(2), 147-159.
Doak, C.C., Doak, L.G., & Root J.H. (1996). Teaching patients with low-literacy skills. Philadelphia: JB Lippincott Co.
Dowse, R., & Ehlers, M.S. (2004). Pictograms for conveying medicine instructions: Comprehension in various South African language groups. South African Journal of Science, 100(11/12), 687-693.
Dowse, R., & Ehlers, M.S. (2005). Medicine labels incorporating pictograms: Do they influence understanding and adherence? Patient Education and Counseling, 58(1), 63-70.
Dowse, R., & Ehlers, M.S. (2003). The influence of education on the interpretation of pharmaceutical pictograms for communicating medicine instructions. International Journal of Pharmacy Practice, 11(1), 11-18.
Dowse, R., & Ehlers, M.S. (2001). The evaluation of pharmaceutical pictograms in a lowliterate South African population. Patient Education and Counseling, 45(2), 87-99.
Programme for Appropriate Technology in Health (PATH) (2002). Developing materials on HIV/AIDS/STIs for low-literate audiences. Family Health International. Retrieved July 8, 2008, from http://www.fhi.org/NR/rdonlyres/e2q7um2s2ffrtcjeesnjqhrgrt4bqawhrjqf
reho2z23rc7lpxiuny3kekvsed4lg3sn5ocrpua3jn/lowlitguide2.pdf.
Fogarty, L., Roter, D., Larson, S., Burke, J., Gillespie, J., & Levy, R. (2002). Patient adherence to HIV medication regimens: A review of published and abstract reports. Patient Education and Counseling, 46(2), 93-108.
Gardner, E.M., Sharma, S., Peng, G., Hullsiek, K.H., Burman, W.J., Macarthur, R.D., et al. (2008). Differential adherence to combination antiretroviral therapy is associated with virological failure with resistance. AIDS, 22(1), 75-82.
Gokah, T.K. (2007). Health education in rural settings in Ghana: a methodological approach. Health Education Research, 22(6), 907-917.
Grimes, J., Blenkinsopp, A., Raynor, D.K., Pollock K., & Knapp, P. (2007). The role and value of written information for patients about individual medicines: a systematic review. Health Expectations, 10(3), 286-298.
USAID. (2008). Programmes Africa. Retrieved July 10, 2008, from the Health Communication Partnership website: http://www.hcpartnership.org/Programmes/Africa/hcp_africa.php.
Houts, P.S., Doak, C.C., Doak, L.G., & Loscalzo, M.J. (2006). The role of pictures in improving health communication: A review of research on attention, comprehension, recall and adherence. Patient Education and Counseling, 61(2), 173-190.
Hugo, J. & Skibbe, A. (1991). Facing visual illiteracy in South African health education: A pilot study. Journal of Audiovisual Media in Medicine, 14, 47-50.
Johnson, A., & Sandford, J. (2005). Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home: Systematic review. Health Education Research, 20(4), 423-429.
Katz, M.G., Kripilani, S., & Weiss, B.D. (2006). Use of pictorial AIDS in medication instructions: A review of the literature. American Journal of Health-System Pharmacy, 63(23), 2391-2397.
Kenny, T., Wilson, R.G., Purves, I.N., Clark, J., Newton, L.D., Newton, D.P., et al. A PIL for every ill? Patient information leaflets (PILs): A review of past, present and future use. Family Practice, 15(5), 471-479.
Kitching, J.B. (1990). Patient information leaflets – the state of the art. Journal of the Royal Society of Medicine, 83(5), 298-300.
Koo, M.M., Krass, I., & Aslani, P. (2003). Factors influencing consumer use of written drug information. Annals of Pharmacotherapy, 37(2), 259-267.
Kwansa, E.V.G., Cannon, J., Belcher, D.W., & Hosu-Porbley, M. (1972). Perception and comprehension of health education visual AIDS by rural Ghanaian villagers. Ghana Medical Journal, 2, 387-396.
Linney B. (1995). Pictures, People and Power. Hong Kong: MacMillan Education.
Maes, A., Foesenek, K., & Hoogwegt, H. (2008). Visual health communication. How do lowliterate audiences understand visual meaning? In: P. Swanepoel, & H. Hoeken. (Eds.), Adapting health communication to cultural needs: Optimizing documents in South African health communication on HIV/AIDS prevention (pp. 151-170). Amsterdam: John Benjamins Publishing Company.
Mansoor, L., & Dowse, R. (2003). Effect of pictograms on readability of patient information materials. Annals of Pharmacotherapy, 37 (July/August), 1003-1009.
Mansoor, L., & Dowse, R. (2006). Medicines information and adherence in HIV/AIDS patients. Journal of Clinical Pharmacy and Therapeutics, 31(1), 7-15.
Mansoor, L., & Dowse, R. (2007). Written medicine information for South African HIV/AIDS patients: Does it enhance understanding of co-trimoxazole therapy? Health Education Research, 22(1), 37-48.
Mathews,C. (2002). Evaluation of a video based health education strategy to improve sexually transmitted disease partner notification in South Africa. Sexually Transmitted Infections, 78(1), 53-57.
Mbizvo, E. Essay theatre – a force for health promotion. Lancet, 368, S30-S31.
Medicines Control Council, Department of Health, Republic of South Africa. (2004).
Guidelines on the requirements for patient information leaflets. Retrieved July 9, 2008, from http://www.mccza.com/documents/2.1420PIL20May04v3.zip.
Mwingira, B., & Dowse, R. (2007). Development of written information for antiretroviral therapy: Comprehension in a Tanzanian population. Pharmacy World & Science, 29(3), 173-182.
National Department of Health, South Africa (2004). National Antiretroviral Treatment Guidelines. Retrieved July 8, 2008, from http://www.doh.gov.za/docs/facts-f.html.
National Work Group on Literacy and Health. (1998). Communicating with patients who have limited literacy skills. The Journal of Family Practice, 46(2), 168-176.
Ngoh, L.N., & Shepherd, M.D. (1997). Design, development and evaluation of visual AIDS for communicating prescription drug instructions to nonliterate patients in rural Cameroon. Patient Education and Counseling, 30(3), 257-70.
Peltzer, K., & Cherian, V.I. (2002). Health promotion on HIV/AIDS in Africa. In: A.O. Alali, & B.A. Jinadu (eds.), Health communication in Africa. Contexts, constraints and lessons (pp. 209-219). New York: University Press of Maerica.
Raynor, D.K., Svarstad, B., Knapp, P., Aslani P., Brooke Rogers, M., Koo, M., et al. (2007). Consumer medication information in the United States, Europe, and Australia: A comparative evaluation. Journal of the American Pharmacists Association, 47(6), 717-724.
Raynor, D.K. (1998). The influence of written information on patient knowledge and adherence to treatment. In, L.B. Myers, & K. Midence, K. (Eds.), Adherence to treatment in medical conditions (pp. 83-112). Amsterdam: OPA/Harwood Academic Publishers.
Schaafsma, E.S., Raynor, D.K., & de Jong-van den Berg, L.T.W. (2003). Accessing medication information by ethnic minorities: Barriers and possible solutions. Pharmacy World & Science, 25(5), 185-90.
Sless, D., & Wiseman, R. (1997). Writing about medicines for people: Usability guidelines for consumer medicines information. 2nd ed. Canberra: Australian Government Publishing Service.
Statistics South Africa (2001). Census 2001. Census in brief. Retrieved July 9, 2008, from http://www.statssa.gov.za/census01/HTML/CInBrief/CIB2001.pdf.
Tripp-Reimer, T., & Afifi, L.A. (1989). Cross-cultural perspectives on patient teaching. Nursing Clinics of North America, 24(3), 613-619.
UNAIDS (2007). AIDS epidemic update. Retrieved July 10, 2008, from http://data.unAIDS.org/pub/EPISlides/2007/2007_epiupdate_en.pdf.
USP DI. Vol. II (2000). Advice for the patient. Drug information in lay language. 20th edition. Englewood, CO: Micromedex.
World Health Organization (2003). Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization.
Zimmerman, M.L. (1982). Instructing through pictures: Print materials for people who do not read. Information Design Journal, 3(2), 119-134.
Appendix
Pictograms in medicines information