ISSA Proceedings 2010 – Argumentation Standards In The Assessment Of Clinical Communication Competence
No comments yet 1. Introduction
1. Introduction
Clinical reasoning, clinical knowledge and clinical skills, which include clinical communication, are essential components of clinical competence recognized internationally in high level policy documents (PSA, 2003; CPMEC, 2006; GMC, 2009). Consequently, communication skills training (CST) has developed as an integral component of medical curricula (Brown, 2008). However, while clinical schools provide general outlines of their CST curricula, content, skills criteria and delivery modes in CST appear to vary across the sector (Bird, Gilbert et al., 2008).
Recently, clinical communication specialists have been calling for new parameters of communication that might draw on inter-disciplinary knowledge and experience to inform how healthcare communication is conceptualised (Skelton, 2008, p.154). In recent work by Gilbert and Whyte (2009; 2010), linguistic and argumentation (viz. critical reasoning) frameworks show how clinical reasoning might be made explicit in communication. The work supports recent perspectives on clinical competence in which not merely expertise in specialised clinical knowledge but also the ability to effectively use clinical knowledge in discourse is regarded as essential (Nguyen, 2006).
In medical education, a student’s ability to effectively integrate content knowledge and clinical reasoning is demonstrated via his/her communication strategy associated with the performance of clinical skills in an oral examination, the Objective Structured Clinical Examination (OSCE). In a conventional OSCE format, a candidate is required to convey medical knowledge and/or demonstrate clinical skills by enacting scenarios with real or simulated patients (viz. actors) or performing specific tasks at several short stations of 8-15 minutes duration. The so-called standardized clinical task is performed under the observation of one or two examiners who score the candidate’s performance on a standardized marking sheet. Thus, the checklist based marking enhances inter-rater consistency and the testing of students’ performances on multiple stations increases the number and range of competencies tested.
Researchers have challenged the ‘objectiveness’ of the OSCE by examining the discourse demands of the clinical assessment context. Roberts, Sarangi et al. (2000) emphasize the mix of discourses – personal experience, professional and institutional – that a candidate must manage in conjunction with the unpredictable interactional demands of the oral examination. Additionally, candidates must simultaneously manage both patient and examiner focussed communication (Gilbert & Whyte, 2009; 2010). Not surprisingly, the discourse tensions of the assessment context challenge the communicative competency of candidates, significantly influencing their strategies of conveying knowledge associated with clinical reasoning and decision-making and, potentially, impacting on their OSCE assessment. As an institutionalised form of assessment, the OSCE potentially serves as a gatekeeper to professional membership (Roberts et al. 2000; Schryer et al., 2003). To gain access to the medical community, novice practitioners, including practitioners from foreign medical cultures, must ‘acquire the rules of assessment as part of their professional repertoire’ (Schryer et al., 2003).
The purpose of the current work is to integrate argumentation standards into CST in order to establish a coherent reference of skills and strategies for aligning the teaching and assessment of clinical reasoning as a component of clinical communication. According to the literature, medical students are rarely taught how to integrate clinical reasoning and communication (Windish, Price et al., 2005). Yet, the practice of medicine is grounded in an oral culture in which decision-making is an essential component of both peer and patient communication. There is growing acknowledgement of the important role that the articulation of logic and critical thinking plays in enhancing clinical encounters and improving patient care (Jenicek & Hitchcock, 2005).
By focusing on communication in OSCEs, the emphasis in the current study is on the complexities of articulating clinical reasoning in oral assessment contexts. In this paper, an overview of the study and the outline of the clinical teaching method will be presented, as the authors evolve a strategy for teaching and analysing the content and structure of arguments used to generate clinical reasoning in the assessment context. The pedagogical approach integrates perspectives on both peer and patient communication and supports students to develop communication strategies that will facilitate their access to membership of the professional community.
2. The Study
In the current study, the model of clinical reasoning and communication proposed by Gilbert and Whyte(2009; 2010) provides the framework for the design and delivery of a program (viz. intervention in the context of the study) concerned with teaching clinical reasoning and communication. The program, referred to as ‘viva voce Clinical Reasoning’, specifically targets the learning needs of Year 3 medical undergraduate students.
Eighteen students have been recruited and allocated into two groups of 9 students by a process of stratified selection (criteria: age; gender; English language at home; repeat students). One group of 9 students is participating in the viva voce Clinical Reasoning program prior to participation in a formative communication assessment task (referred to as a ‘mock’ OSCE or MOSCE). In the formative assessments, one set of examiners (E1 and E2) will rate the students’ knowledge and communication using assessment criteria similar to those used in standard OSCE assessments and the other set of examiners (E3 and E4) will rate the students’ knowledge and communication using assessment criteria that specifically measure components of argument and reasoning, consistent with the frameworks established for the program’s teaching. Simulated patients will rate the students’ apparent effectiveness of communication using a brief evaluation instrument. The results of both groups of students will be compared.
At the time of writing, the intervention phase of the study is completed with the evaluation to take place in late August, 2010. The primary outcome measure of the intervention will be the two formative assessment tasks which students will undertake at the university medical school site. Hence, the focus of this paper will be on outlining the argumentation frameworks which inform the design of the teaching intervention and assessment frameworks. We believe that this is an innovative approach to clinical communication skills training and that the materials evolved for the program, which rest on argumentation principles, should be of special interest to those working in health communication and also to argumentation scholars interested in broadening the applications of critical reasoning and argument to disciplines outside the traditional philosophy domains.
3. The Intervention: viva voce Clinical Reasoning Program
3.1. Theoretical framework
The primary objective of the program is to teach students strategies for effectively communicating their clinical reasoning and decision-making in clinical assessment contexts. Making explicit the tacit rules of clinical reasoning is important for professional acculturation and the development of professional expertise in clinical contexts. The model of argument for clinical practice proposed by Gilbert and Whyte (2009; forthcoming) has been used to design the framework for a program called the viva voce Clinical Reasoning program, which aligns the teaching and assessment of clinical reasoning as a component of clinical communication. In this model of clinical communication, clinical practice falls into diagnostic and therapeutic domains and is defined in terms of the core skills of diagnosis, management and counselling. Diagnosis, management and counselling are each typified by primary communicative goals. Arguments used for inquiry, justification and persuasion are sketched in the diagnosis, counselling and management contexts of clinical practice and arguments are used to generate reasons which support the communicative goals associated with the essential skills of clinical practice (Gilbert & Whyte, 2009; 2010). The focus of the model is on aligning communicative goals of clinical practice contexts with professional competency standards of the profession (i.e. what doctors are expected to perform in practice) with an emphasis on the effectiveness of communication on clinical outcomes.
3.2. Learning objectives
Argumentation and linguistic theories underpin the program’s learning objectives, and students who complete the program should be able to:
- a. Reconceptualise clinical communication as an argument-based activity, considering the differences between diagnostic determination and therapeutic decision-making;
- b. Recognise and begin to apply RSA (relevance, sufficiency, acceptability) criteria of argument standard;
- c. Recognise and accommodate biomedical beliefs and socio-cultural experiences in doctor-patient reasoning strategies;
- d. Develop effective strategies for communicating provisional diagnoses and differential diagnoses and for outlining a problem prioritisation;
- e. Recognise the defining communication characteristics of informed consent: negotiation, concordance, compliance;
- f. Recognise potential biases in therapeutic decision-making;
- g. Recognise the communication goal of a given OSCE and describe appropriate predictive moves/stages necessary for organising the discourse;
- h. Select appropriate language for communicating to an examiner (or colleague) relevant issues considered in diagnostic determination; and
- i. Elicit and deliver relevant clinical content under the time constraints of an OSCE.
3.3 Program synopsis
The pilot study was approved by the Monash University Human Research Ethics Committee. Two 2-hour workshops were approved for delivery. Ideally, a longer series of workshops was desirable but it was important that the study did not impose on the students’ current workloads and timetable commitments. Medical students at Monash commence their clinical placements in third year. Owing to the time limitations as well as the learning stages of the students, and after consultation with the relevant clinical school coordinators, it was decided that the focus of the viva voce Clinical Reasoning program should be limited to diagnostic reasoning, as this would best accommodate the students’ existing learning needs within the context of their curriculum. Therapeutic reasoning, as accommodated in the model, would be better addressed at higher year levels and with more time allocated for program delivery.
The two workshops integrated instruction, practice, feedback and modelling to promote interactive, experiential and reflective processes for students. Although doctor-patient communication was identified as an essential component of the OSCE scenarios, the emphasis in teaching was on intra- and inter-professional communication.
The learning objectives were reformulated to make the important concepts of diagnostic reasoning more accessible for the students so that after the program, students could expect to be able to:
- a. Expand possible causes for patient symptoms (and signs) in an organised way;
- b. Collect evidence to support or deny diagnostic possibilities (for common and/or important surgical and medical problems) using history, examination and investigations;
- c. Demonstrate reasoning in the consultation process;
- d. Marshall evidence to tell a defensible medical story (anticipate challenges); and communicate diagnostic outcome(s) and recommended action to both medical and patient audiences.
The outlines of the two workshops are sketched below. At the first workshop, some of the concepts of clinical reasoning were unpacked for students and strategies for communicating clinical reasoning effectively within the time constraints of an oral clinical assessment task were considered. The emphasis was on marshalling evidence to support a provisonal diagnosis and on defending it from potential challenges (i.e. to demonstrate the student’s knowledge of other less likely but still valid diagnostic possibilities). At the second workshop, students were provided with opportunities to put into practice specific communication strategies using mock assessment tasks (MOSCEs) with structured feedback/assessment guidelines.
Workshop 1 Outline
Part 1: Introduction
General outline on the use of reasoning (viz. ‘arguments’) in clinical communication (diagnostic/therapeutic practice)
A focus on the articulation of reasoning in clinical assessment
Part 2: History-taking as Inquiry
Emphasis on focussed data gathering that narrows the options
Part 3: Diagnostic Formulation and Decision-making
Establishing a provisional diagnosis
Building the differential diagnosis
The use of ‘defining’ and ‘discriminating’ features in communicating clinical diagnosis
Developing the problem prioritisation
Diagnostic certainty and uncertainty
Part 4: Investigations as Support for Diagnosis and Management Strategy
Workshop 2 Outline
Part 5: Clinical Assessment (OSCE) and the Communication of Reasoning
Organisation of reasoning in OSCEs (predictive moves/stages)
Assessment/feedback frameworks to guide recommended communication strategy
Language of reasoning in OSCEs (semantic qualifiers; transition signals)
Elicitation and delivery of relevant content under time constraints
Part 6: Trial OSCEs (practice scenarios)
4. Argumentation Frameworks used to Teach Clinical Reasoning
Students were presented with clinical scenarios, similar to the OSCE format. Each scenario was designed to be of ten minutes total duration (eight-minute task plus two-minute reading time). Working in small groups of two to three, students rotated the roles of a) simulated patient, b) candidate, and c) examiner in the scenarios to practice the communication strategies and to deliver structured and specific feedback.
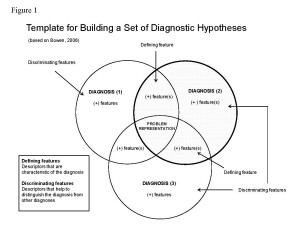
Before commencing the role play, students were asked to consider the task and begin a diagnostic hypothesis. The students were provided with a template for building a set of diagnostic hypotheses (refer to Figure 1). As previously illustrated by Gilbert and Whyte (2009, forthcoming), the dialectical tier of argument is subtly constructed in medical discourse. Semantic qualifiers are terms selected to articulate clinical reasoning. Descriptors used to characterise the diagnosis are referred to as defining features and descriptors used to distinguish the diagnoses from one another are referred to as discriminating features. The use of semantic qualifiers provides an efficient linguistic strategy for comparing and contrasting diagnostic considerations (Bowen, 2006: 2219). The most-likely diagnosis is formulated during the clinical reasoning process while the options of differential diagnosis are subtly discounted.
Students were presented with the following clinical scenario:
Mrs WM presents to your surgery with a pain in her chest that makes it difficult to cough. She is 65 years old and has been unwell for the last three days.
You have 5 minutes to take a history, after which you will be asked some questions about likely diagnoses and investigations.
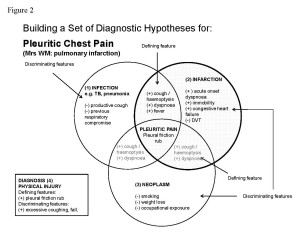
A set of diagnostic hypotheses were established and summarised in the template provided for the scenario (refer to Figure 2).
A strategy for organising the discourse in the setting of an OSCE was then outlined. This required the students to recognise the communication goal of the OSCE; in this case, to communicate a diagnostic work-up and diagnostic decision while taking a patient history. The students were then shown how to effectively organise the discourse into predictive moves or stages, equipping them with a strategy for efficiently communicating the diagnostic decision (after taking a patient history) while simultaneously articulating the diagnostic options in the development of a dialectical tier. This required the students to select appropriate semantic qualifiers to emphasise the discriminatory features of illness. Students needed to be familiar with the linguistic descriptors for relevant positive and relevant negative defining and discriminating features of illness.
The following example transcript was provided to students after the task, as a model for practice. Not intended to be prescriptive but merely a guide for practice, the transcript is divided into predictive stages/sequences so that students may realise the benefits of strategically organising language and discourse in the communication of clinical reasoning. The challenge for the students was to achieve this during the process of history-taking. While students may not know the diagnostic decision at the outset of the simulated consultation, they would expect their summative OSCE assessment at the end of the year to have a range of common and/or important medical and surgical problems and so should be capable of surmising on diagnostic options early in the scenario and then be able to narrow down the available options during the course of history-taking.
The model transcript, below, illustrates predictive stages of a history-taking OSCE station. In Stages 3 and 4, the defining and discriminating descriptors are italicised, to show the importance of these linguistic items in communicating diagnostic deliberation.
Model Transcript 1
[Stage 1: Establishing the problem representation (pleuritic pain and cough)]
1 Doctor: Good morning, Mrs Martin, what has brought you to the clinic today?
2 Mrs Martin: I have a very bad pain in my chest, which has been there for about three days now and it doesn’t seem to be getting any better.
3 Doctor: Can you describe the pain?
4 Mrs Martin: Well, it’s a terribly sharp pain here on my right side, and it hurts mostly when I cough or sneeze.
5 Doctor: Have you tried anything to relieve the pain?
6 Mrs Martin: Oh yes, I if I try to hold my breath, then the pain feels a lot better.But that’s not very comfortable to do. So, I also put my hand firmly on my chest over the pain and that makes it feel a little better. I’ve tried some pain-killers and they also help a bit.
7 Doctor: Do you get pain anywhere else?
8 Mrs Martin: No, just here over the same spot.
[Stage 2: Announcement of diagnostic deliberation: Intention to conduct inquiry]
9 Doctor: Are you experiencing any other symptoms or discomfort?
[Stage 3: Elaboration of the problem representation: Focus on defining features]
10 Mrs Martin: Yes, I started coughing about three days ago. You see, this all started by me feeling unwell with a cough and mild fever.
11 Doctor: Is it a dry or productive cough?
12 Mrs Martin: Generally, it’s a dry cough. But, when it started, I was bringing up a little bit of sputum.
13 Doctor: Did you notice any blood in your sputum?
14 Mrs Martin: Yes, just a very little bit on the first day, but only once and so I didn’t get too worried about it.
15 Doctor: Is your cough getting any better now?
16 Mrs Martin: I think my cough is feeling better but even a slight cough upsets my chest pain. I am tired of it.
[Stage 4: Articulation of diagnostic options: Focus on discriminatory features]
[Diagnostic Option 1: Infarction]
17 Doctor: Have you experienced any shortness of breath or difficulty breathing?
18 Mrs Martin: Around the time of the pain starting, I told you I also had a fever. Well, I was feeling a little breathless at the time, too, and quite a shortness of breath overcame me on the first day so that I had to lie down and take a rest until I felt my breathing get more normal again. Only for about an hour or so was it like that. Now, I’m still feeling a little more breathless than usual.
19 Doctor: Have you recently had a period of prolonged rest or immobility?
20 Mrs Martin: Yes, about two weeks ago I sprained my ankle in the garden and so I spent five days resting on the couch at home. My ankle is pretty good right now.
21 Doctor: Do you have a history of heart failure or DVT?
22 Mrs Martin: The doctor says I have heart failure but I don’t feel too much affected. Sometimes, I notice that my ankles swell a bit, and that’s somehow related. But, I don’t think it is all that bad. I’m on medication for it.
[Diagnostic Option 2: Infection]
23 Doctor: Do you have a history of chest problems?
24 Mrs Martin: No
[Diagnostic Option 3 : Neoplasm]
25 Doctor: Have you noticed any change in your weight?
26 Mrs Martin: No, I have been more or less the same weight for the last five years.
27 Doctor: Have you ever smoked?
28 Mrs Martin: No.
29 Doctor: Can you tell me about your work history?
30 Mrs Martin: I was an accountant but retired five years ago so that my husband and I could enjoy ourselves a bit and spend time with our two grandchildren.
Students were also shown strategies for explaining their diagnostic decisions, responding to prompts by the examiner. The following model transcript illustrates a strategy for stating a diagnostic decision, articulating the potential challenges to that decision, and providing suitable rebuttals to discount those challenges. The use of appropriate semantic qualifiers to describe evidence of symptoms and signs is, once again, crucial.
A model transcript illustrating a strategy for articulating and defending a diagnostic decision is shown below. In this transcript, evidence for supporting the diagnostic decision is clearly stated. Diagnostic options are identified but relevant negative symptoms and signs are articulated to discount them as most likely diagnosis.
Model Transcript 2
[Articulation of provisional diagnosis: Diagnostic decision]
Examiner: Can you provide a likely diagnosis for Mrs Martin’s problem?
Candidate: My provisional diagnosis is pulmonary infarction secondary to a pulmonary embolism.
[Articulation of differential diagnosis: Potential challenges to decision]
Examiner: What evidence supports your diagnosis?
Candidate: Mrs Martin’s acute onset of dyspnoea, haemoptysis and her recent immobility support a diagnosis of pulmonary infarction secondary to pulmonary embolus. Her history of congestive heart failure is also significant.
Examiner: What other diagnoses might you consider and why?
Candidate: Mrs Martin might have a lung infection, as she reports having a mild fever. However, fever may sometimes occur in the presence of pulmonary embolism. Mrs Martin does not show other signs to support the diagnosis of infection e.g. productive cough, previous respiratory compromise.
Pleuritic pain may be associated with a neoplasm. However, Mrs Martin has never smoked, denies weight loss and reports no exposure to cancer-causing substances. Hence, this diagnosis seems unlikely.
Finally, the students were advised on strategies for organising their discourse for an oral case presentation format, a regular requirement of assessment and work-based learning. The following model of case presentation summary was provided with relevant moves marked in the discourse to illustrate an efficient strategy for organising language and reasoning. Once more, the defining and discriminating features are italicised to show the importance of these linguistic items in communicating diagnostic deliberation.
Model Transcript 3 Case Presentation Summary
[Defining features: Problem representation]
Mrs Martin has presented with a stabbing right-sided chest pain that is especially severe when she breathes, coughs, or sneezes. It is relieved by holding her breath or exerting pressure against the affected chest. The pain has been present for about three days; although it is not getting worse it has also not improved very much. The pain is localised and does not radiate.
[Discriminating features: Diagnosis 1 Infarction]
Mrs Martin felt unwell three days ago when she experienced an episode of acute dyspnoea and subsequently developed a mild low-grade fever and cough. She initially coughed up some blood-stained sputum, but only once and not enough to make her feel too alarmed. Her cough has improved slightly but Mrs Martin reports that even mild coughing aggravates her chest pain enough to cause her significant distress. She finds breathing difficult. Two weeks ago, Mrs Martin sprained her ankle and spent about five days relatively immobile, resting on the couch at home. Mrs WM has a history of congestive cardiac failure (CCF) but has no history of deep vein thrombosis (DVT).
[Diagnosis 2: Infection]
Mrs WM’s cough is generally non-productive and she has not experienced any recent respiratory illness.
[Diagnosis 3: Neoplasm]
Mrs WM does not smoke and reports no recent loss of weight. She worked as an accountant until 5 years ago, when she retired. She now lives at home with her husband.
[Articulation of diagnostic decision]
Mrs Martin’s acute onset of dyspnoea, haemoptysis and her recent immobility support a diagnosis of pulmonary infarction secondary to pulmonary embolus. Her history of congestive heart failure is also significant.
[Articulation of diagnostic options]
[Option 1]
Mrs Martin might have a lung infection, as she reports having a mild fever. However, fever may sometimes occur in the presence of pulmonary embolism. Mrs Martin does not show other signs to support the diagnosis of infection e.g. productive cough, previous respiratory compromise.
[Option 2]
Pleuritic pain may be associated with a neoplasm. However, Mrs Martin has never smoked, denies weight loss and reports no exposure to cancer-causing substances. Hence, this diagnosis seems unlikely.
5. Argument Frameworks used for the Assessment of Clinical Reasoning
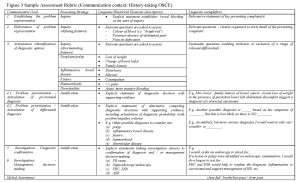
Assessment and feedback rubrics were designed by integrating argument components into the communication frameworks (aligned with the teaching strategies discussed in section 4, above). Students were shown how to use these to guide their feedback to each other during the role play practice.
Figure 3 is an example of one of the assessment rubrics developed for the course on the topic of rectal bleeding. Clinical content is embedded in reasoning strategy to support the communicative goals at each stage of the clinical scenario. Students were encouraged to articulate their decision-making and were advised on suitable discourse and linguistic structures to support and effective communication strategy for their oral assessment tasks (viz. OSCE).
6. Conclusion
In summary, we believe the viva voce Clinical Reasoning program, by integrating principles of argumentation theory and clinical reasoning into a communication concept, offers an innovative approach to clinical communication skills training. Concepts from argumentation and principles of discourse analysis underpin the strategy. The teaching methods and resources along with the assessment rubrics represent a novel approach to clinical communication skills training. Preliminary feedback from the students attending the program reveals their enthusiasm for explicit instruction on how to communicate their reasoning effectively in the assessment context of an OSCE. All students attending the workshops reported never having received explicit instruction on how to build a case for diagnostic determination (albeit Year 3 students with half a year on the wards) and expressed a strong appreciation of the linguistic strategies and resources as well as the notions of argument that were built into the instruction. Further analysis of the data once data collection is complete is expected to reveal the impact on such instruction on students’ communication strategies and assessment outcomes. It is intended to use the results to inform medical curriculum and assessment across both third and fourth years of the medical course.
REFERENCES
Bird, B., Gilbert, K., Jolly, B., Spike, N., & Kiegaldie, D. (2008). Challenges faced by International Medical Graduates in the VMA Training Program: Final Report to the Victorian Metropolitan Alliance. June, 2008. Melbourne: Faculty of Medicine, Nursing and Health Sciences, Monash University.
Bowen, J.L. (2006). Educational strategies to promote clinical diagnostic reasoning. New England Journal of Medicine, 355(21), 2217-2225.
Brown, J. (2008). How clinical communication has become a core part of medical education in the UK. Medical Education, 42, 271-278.
Confederation of Postgraduate Medical Education Councils (CPMEC) (2006). Australian Curriculum Framework for Junior Doctors (version 2.1). Accessed July 2010 at: http://curriculum.medeserv.com.au/Curriculumv2.1_A4.pdf
General Medical Council (GMC) (2009). Tomorrow’s Doctors: Outcomes and Standards for Undergraduate Medical Education. London: GMC. Accessed September 2009 at: www.gmc-uk.org/education/undergraduate/tomorrows_doctors_2009.asp
Gilbert, K., & Whyte, G. (2009). Argument and medicine: A model of reasoning for clinical practice. In J. Ritola (Ed.), Argument Cultures. Conference proceedings of the 8th Ontario Society for the Study of Argumentation (OSSA) Conference [CD]. University of Windsor: OSSA.
Gilbert, K., & Whyte, G. (forthcoming). The use of arguments in medicine: A model of reasoning for enhancing clinical communication. Monash University Linguistics Papers (MULP) [revised version of OSSA2009 paper]
Jenicek M., & Hitchcock, D.L. (2005). Logic and Critical Thinking in Medicine. American Medical Association Press.
Nguyen H.T. (2006). Consulting ‘expertness’: A novice pharmacist’s development of interactional competence in patient consultations. Communication & Medicine, 3(2), 147-160.
Pharmaceutical Society of Australia (PSA) (2003). Competency Standards for Pharmacists in Australia 2003. Accessed November 2008 at: http://www.psa.org.au/site.php?id=643
Roberts C., S.Sarangi, L. Southgate, R. Wakeford, & V. Wass (2000). Oral examinations – equal opportunities, ethnicity, and fairness in the MRCGP. British Medical Journal, 320(7231), 370-74.
Schryer CF, Lingard L, Spafford M, & Garwood K. (2003). Structure and agency in medical case presentations. In: Bazerman C, Russell DR. (Eds.), Writing Selves/Writing Societies. Colorado State University: WAC Clearinghouse.
Windish, D.M., Price, E.G., Clever, S.L., Magaziner, J.L., & Thomas, P.D. (2005). Teaching medical students the important connection between communication and clinical reasoning. Journal of General Internal Medicine, 20 (11).
You May Also Like
Comments
Leave a Reply